Healthcare System Integration with Boomi: Connecting EHR, Labs, Billing, and Analytics
Healthcare organizations operate in environments where multiple systems must exchange data continuously and reliably. Clinical workflows, laboratory operations, billing processes, insurance validation, and analytics all depend on accurate and timely data movement across platforms. Most healthcare integration issues do not appear during initial implementation. Systems connect, data flows are tested, and early results seem stable. Problems usually surface later, when transaction volumes increase, workflows change, or new systems are introduced. At that point, system integration becomes an operational dependency rather than a technical detail. Industry standards help align data formats, but they do not solve orchestration, monitoring, and long-term reliability. As healthcare platforms scale, the way healthcare system integration is structured determines whether growth leads to stability or recurring operational friction.
The Reality of Healthcare System Landscapes
A typical healthcare technology landscape includes a mix of systems implemented at different times and sourced from different vendors. Common system categories include:
- Electronic Health Records (EHR / EMR)
- Laboratory Information Systems (LIS)
- Billing and claims platforms
- Insurance eligibility and clearinghouse services
- Business intelligence and analytics tools
Each system is designed to solve a specific problem and evolves independently. Updates, regulatory changes, and vendor roadmaps rarely align. This creates constant pressure on data integration in healthcare, which must adapt without disrupting operations.
Fragmentation itself is not unusual in healthcare. The risk appears when integrations are implemented as isolated point-to-point connections without a centralized approach to integration architecture.
Organizations addressing this challenge often rely on Boomi Integration services combined with Dedicated Development Teams to ensure integrations evolve alongside core systems and business requirements.
Where Integration Friction Starts
Integration friction typically arises from mismatched system priorities:
- Clinical systems focus on accuracy and completeness
- Billing systems focus on reconciliation and timeliness
- Insurance services depend on external response cycles and validation rules
- Analytics platforms require consistent, structured datasets
Standards such as HL7 FHIR interoperability standards and guidance from HealthIT.gov on FHIR adoption help normalize how healthcare data is represented and exchanged through APIs.
However, standards alone do not manage how data moves across multiple systems over time. Orchestration, retries, partial failures, and change management still require a dedicated healthcare integration platform.
Industry research from HIMSS on healthcare interoperability consistently frames interoperability as an ongoing operational responsibility rather than a one-time technical milestone.
Common Integration Challenges by System Type
Individually, these challenges are manageable. Together, they create environments where healthcare data integration requires constant oversight and manual intervention.
Why Point-to-Point Integrations Fail Over Time
Point-to-point integrations are often chosen because they are fast to implement and easy to understand. Their limitations become visible as systems scale.
Each new connection introduces additional dependencies. A single system change can impact multiple downstream integrations. Over time, the integration landscape becomes fragile and difficult to maintain.
Common failure patterns include:
- Integration logic spread across multiple systems
- Inconsistent error handling
- Limited visibility into data flow failures
- Reliance on individual developers or undocumented knowledge
Failures are frequently silent. Data may arrive late, partially, or not at all, without triggering alerts. Issues are often discovered through reporting discrepancies or operational delays rather than system notifications.
This accumulation of manual workarounds and hidden failures is commonly described as integration technical debt.
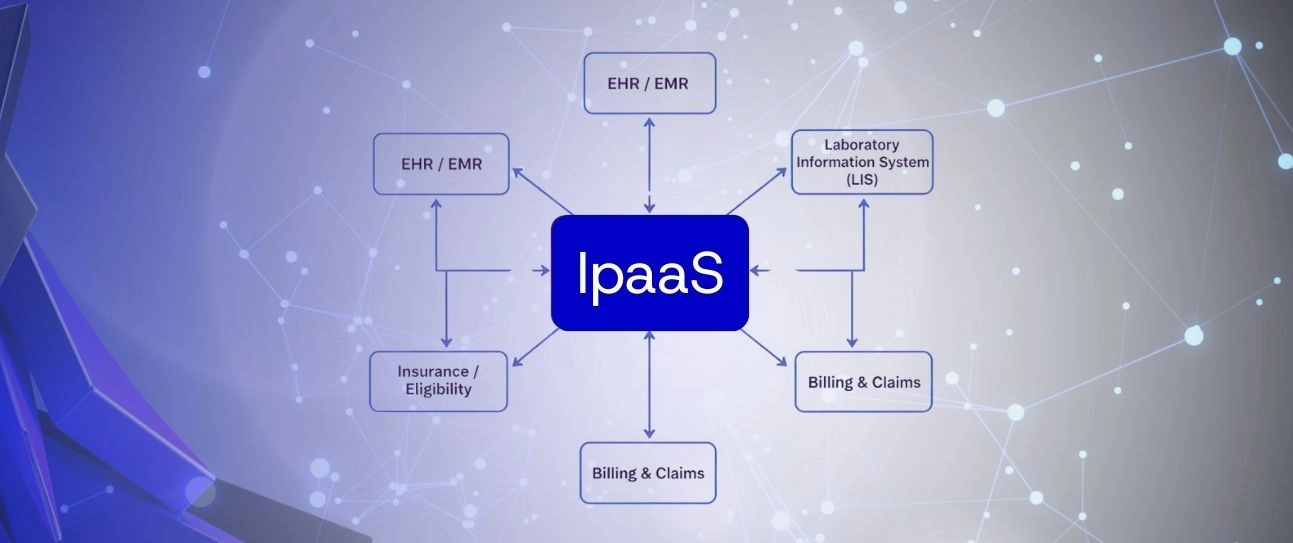
iPaaS as an Integration Control Layer
An Integration Platform as a Service (iPaaS) introduces a centralized model for managing how systems interact. Instead of embedding integration logic directly into each system-to-system connection, integrations are routed through a managed layer.
This layer typically handles:
- Data mapping and transformation
- Multi-step workflow orchestration
- Error handling and retry logic
- Monitoring and operational visibility
- Controlled changes across environments
Platforms such as Boomi iPaaS platform are commonly used to implement this model in healthcare environments, where integration reliability, data traceability, and operational visibility are critical.
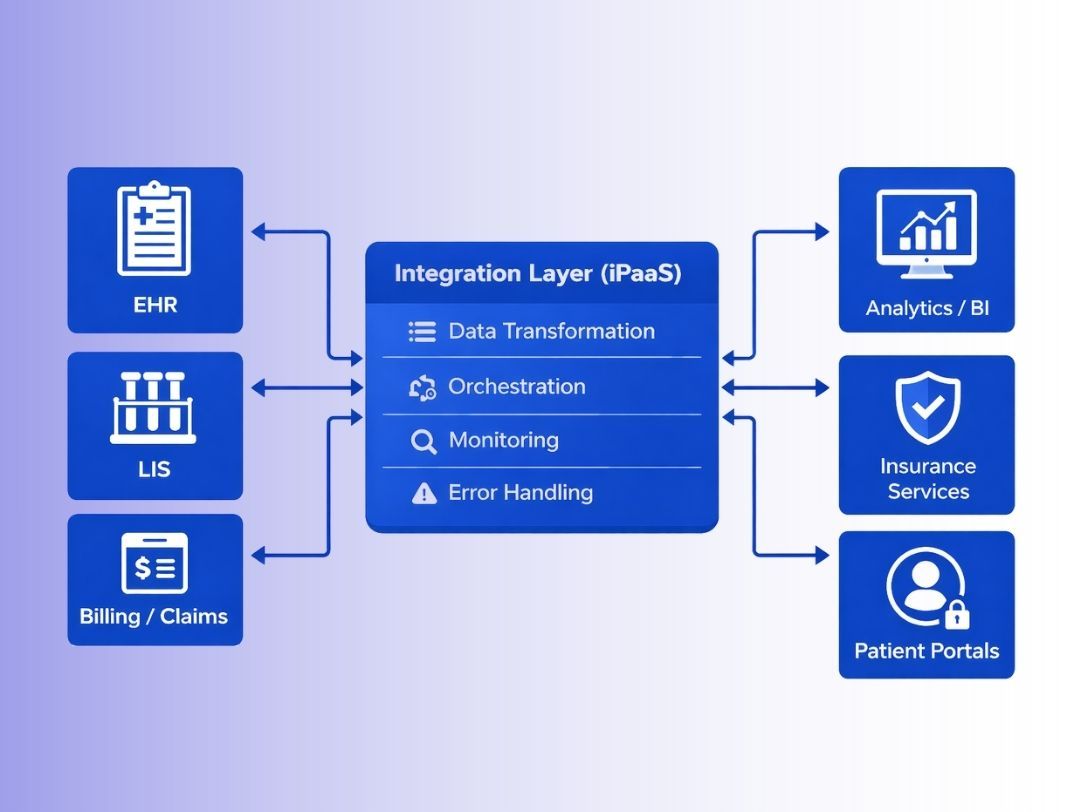
healthcare-ipaas-integration-layer-diagram
Integration Architecture Checkpoint
Organizations planning to scale healthcare platforms, onboard new partners, or expand reporting capabilities often benefit from reviewing how integrations are currently structured and where operational risk may be accumulating.
If you are evaluating healthcare integration architecture or planning changes, you can contact Bluepes integration experts to discuss integration strategy and implementation options.
Practical Integration Patterns in Healthcare
Healthcare integrations rarely operate as simple one-to-one connections. In practice, most workflows involve multiple systems reacting to the same event.
A common example is EHR-driven integration flows, where a clinical event triggers updates across billing, insurance, and analytics systems. Another frequent pattern is lab result distribution, where results must be delivered reliably to EHRs, reporting platforms, and downstream clinical systems.
These scenarios require orchestration, sequencing, and conditional logic rather than simple data transfer. This is where event-driven healthcare integration becomes essential, allowing systems to react consistently to changes without tight coupling.
Integrating EHR, Labs, Billing, and Analytics with Boomi
In healthcare environments, integration flows often follow repeatable architectural patterns:
- EHR publishes patient or encounter updates
- LIS sends lab results as events
- Billing systems consume validated clinical data
- Analytics platforms receive structured datasets
Using a centralized Boomi integration platform allows these flows to be managed as reusable processes rather than isolated connections.
This approach supports:
- Standardized data transformations
- Controlled sequencing of dependent steps
- Retry logic for partial failures
- Clear separation between systems and integration logic
As a result, healthcare system integration becomes easier to maintain and adapt as systems evolve.
Monitoring, Traceability, and Operational Visibility
One of the most overlooked aspects of healthcare data integration is observability. Many integration failures do not result in system outages. Instead, data arrives late, partially, or inconsistently.
Effective integration architectures include:
- End-to-end process monitoring
- Centralized logging
- Clear error classification
- Alerts aligned with operational impact
Without visibility, teams often rely on manual checks or downstream reporting issues to detect problems. This delays response times and increases operational risk.
Modern integration platforms support integration monitoring and traceability, allowing teams to identify where data stopped moving, which system caused the issue, and what corrective action is required.
Managing Change Without Breaking Integrations
Healthcare systems are continuously updated. Vendors release new versions, regulatory requirements change, and internal workflows evolve.
Without a structured integration layer, each change introduces risk. Point-to-point integrations require updates across multiple connections, increasing the chance of regression.
A centralized integration architecture for healthcare allows teams to:
- Isolate changes to specific integration processes
- Test updates independently
- Maintain backward compatibility
- Reduce dependency on individual developers
This capability is critical for long-term platform stability.
Scaling Healthcare Platforms Without Rebuilding Integrations
As healthcare organizations grow, integration complexity grows with them. New clinics, new partners, new reporting needs, and new digital services all depend on reliable data exchange.
Scalable healthcare integration platforms make it possible to:
- Add systems without redesigning existing flows
- Reuse integration logic across environments
- Maintain consistent behavior under higher loads
This is especially relevant for organizations operating across regions or expanding service portfolios.
Teams supporting these initiatives often combine platform expertise with ongoing engineering support through Dedicated Development Teams to ensure integrations remain stable as the business scales.
Conclusion
Healthcare integration challenges are not caused by a lack of systems or standards. They are caused by unmanaged complexity as systems evolve independently over time.
Treating healthcare system integration as infrastructure rather than a one-time project improves reliability, visibility, and operational confidence. Centralized integration platforms such as Boomi support this model by providing control over how data flows, how failures are handled, and how change is managed.
Organizations that invest in structured healthcare integration architecture reduce long-term operational risk and create a more stable foundation for growth.
If you are planning to scale healthcare platforms, integrate new systems, or improve integration reliability, reviewing your current integration architecture is a practical first step.
You can contact Bluepes Boomi integration specialists to discuss healthcare integration challenges and possible implementation approaches.
Interesting For You
Why Businesses Are Rethinking Integrations (And What They’re Doing Instead)
The Hidden Problem Slowing Companies Down Most businesses don’t think about integrations—until something goes wrong. A new CRM rolls out, but customer data doesn’t sync. Finance can’t generate accurate reports because revenue numbers are off. An ERP upgrade breaks existing workflows. Every company depends on multiple tools—ERP, CRM, supply chain software, cloud storage, payroll systems—but getting them to work together? That’s where things fall apart. 📌 Missed revenue opportunities because data is delayed or incomplete. 📌 IT teams overloaded with patching broken connections. 📌 Security risks from outdated APIs and manual data transfers. For years, businesses have tried three main approaches to integration—but each comes with serious trade-offs.
Read article

How Boomi Accelerates Cloud Transformation in Regulated Industries
Cloud transformation is no longer a question of “if” — it’s “how fast and how safely.” But for businesses operating in regulated environments, speed is only part of the equation. Compliance, security, and auditability shape every decision. Healthcare. Financial services. Legal tech. These are not industries where you can simply plug in new tools and move on. Data is sensitive. Processes are scrutinized. Mistakes are expensive. This is why more organizations in highly regulated sectors are turning to Boomi.
Read article

Hybrid Integration Architecture with Boomi: Building Resilience Across Cloud and On-Prem Systems
Enterprises rarely run entirely in the cloud. Critical data still resides in legacy databases, ERP systems, and on-prem applications that cannot easily migrate. A hybrid integration architecture allows organizations to connect both worlds - combining the flexibility of cloud services with the reliability of local infrastructure. Boomi’s platform plays a central role in this setup. It supports secure, event-based communication between on-prem and cloud systems, enabling real-time data exchange without compromising governance or performance. This article outlines how hybrid integration works in practice, the architecture patterns it uses, and the benefits it brings to modern enterprises.
Read article